Promised Health Care Comes Too Late For Some Guest Workers in Canada
By Dominique L. Johnson
Cronkite Borderlands Initiative
TORONTO — When Winston Morrison came to Ontario as a guest worker nine years ago, he expected to provide a better future for his family in Jamaica. He didn’t expect to lose his leg.
Nor did he expect the initial reluctance of the Canadian government to pay for his extensive medical care since guest workers in the Seasonal Agricultural Worker Program are eligible for health care coverage the day they arrive in the country.
Yet when asked if he would recommend that other Jamaicans sign up for Canada’s guest worker program, Morrison gives an unexpected answer.
“This program is really helpful because it puts food in lots of people — because you have one farm worker, who maybe feeds like 30, 40 different people," said Morrison. "I take care of my kids, and maybe my mom, my common-law wife, and maybe somebody in this family get benefits, somebody in that family get benefits. It stretches so far."
Still, Morrison has a warning for his fellow guest workers: “I would encourage them, when you come, do your best, but know your rights."
Morrison’s case illustrates both the dangers of farm work and the benefits of having guest workers covered by a health care program. As the U.S. Congress debates a guest worker program as part of national immigration reform, it remains unclear what health care would be provided to temporary workers. While some proposals would mandate worker’s compensation insurance, virtually none would require health care insurance for farm workers despite some sobering statistics.
In the U.S., working on farms or ranches is the fourth most dangerous job in the nation in terms of fatalities, according to a 2010 U.S. Bureau of Labor Statistics report.
A 2013 report released by the Kresge Foundation, a Troy, Mich.-based group dedicated to helping low-income people, underscores that point. It found that people employed as farm workers in the U.S. were five times more likely to have a fatal occupational injury than were workers in all civilian industries combined.
Yet an estimated 75 percent of U.S. farm workers — the vast majority of whom are undocumented — aren’t covered by health insurance, according to the Kresge Foundation report.
That isn’t the case in Canada, which the United Nations has lauded as a model guest worker program for the safeguards it provides to workers.
Workers in the SAWP, established in 1966, are covered by health insurance the day they arrive in Canada until the day they return to home. They get the same healthcare plan that covers Canadian citizens in the province where they are employed.
In Ontario, the province with the largest number of seasonal agricultural employees — 28,845 — workers are covered under the Ontario Health Insurance Plan. Employers who contract for guest workers pay for their health insurance. There is no cost to the workers.
Guest agricultural workers in a newer program, the Temporary Foreign Worker Program, must wait three months before they qualify for the province’s healthcare plan. During the waiting period, they receive private health coverage through their employer.
Despite the near universal coverage, critics say that guest workers don’t always take advantage of the health care benefits because they fear doing so may put them in a negative light with their employers.
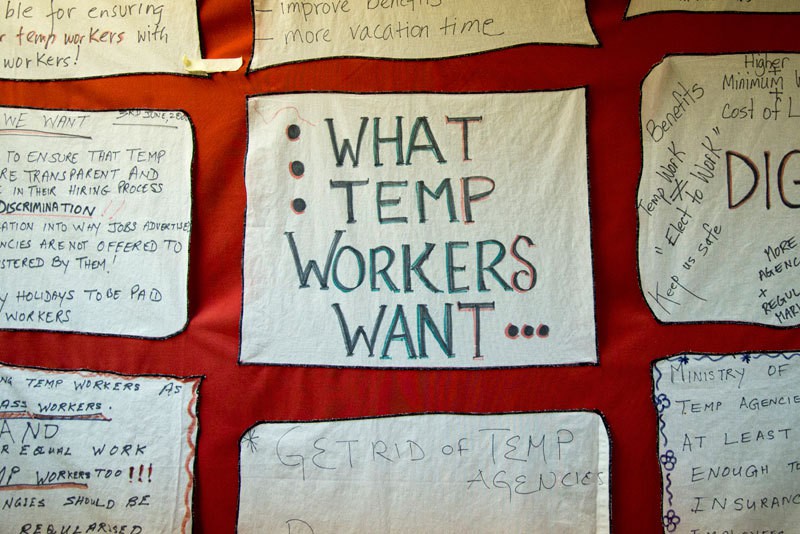
“A lot of them do get ill because the work they do is so arduous, and takes such a toll on the bodies that the last thing many of them want to do is bring any attention to any type of injury they may have or any problems with their body, even a toothache,” said Evelyn Encalada Grez, co-founder of Justicia 4 Migrant Workers, an Ontario-based farm worker rights advocacy group. “They don’t want employers to see them as being defective in any way…and they don’t want to be seen as slowing down production.”
However, Ken Forth, a farmer and president of Foreign Agricultural Resource Management Services, which administers the seasonal worker program in Ontario, argues the success of Canada’s seasonal program is due to the strict scrutiny and safeguards built into the program.
Claims that a worker would keep quiet on an injury or not report any health problems to the program are not credible with Forth. He said the program includes regular meetings with home country representatives to air grievances and work out problems.

Winston Morrison, 38, from Jamaica, talks about his experiences as a guest worker in Canada. In 2011, Morrison fell and injured his right knee while spraying pesticides in a greenhouse. An infection developed in his injured knee that later required amputation of his leg. Photo by Lillian Reid. |
“We go to annual review meetings of this program with all those countries' representatives, the workers’ representatives, the liaison services," Forth said. "Are there some issues? Sometimes, but most of it is all positive stuff, and we move forward. There’s checks and balances here."
Forth said a worker with a problem can dial their liaison to get help.
"To say that they’re afraid, I don’t get that one," Forth said. "I don’t see anybody being afraid — at least my guys aren’t afraid."
And Forth said not attending to a worker’s medical needs isn’t good for the overall farm operations.
“A worker that’s not happy in his workplace or injured in his workplace — how productive do they think that is? Farmers are all about productivity,” Forth said.
“I mean, if you have a tractor that’s broke down and doesn’t work, how much productivity is there? If you have a worker that’s injured, how much productivity is there?”
While Forth contends that workers would seek health care and employers wouldn’t risk being suspended from the program for mistreating workers, researchers, like Dr. Janet McLaughlin of Wilfrid Laurier University in Brantford, Ontario, said the workers’ fears of being sent home or “repatriated” for complaining is real.
“With respect to their work contracts, they have very little power to change negative circumstances because the contracts are typically tied to an employer, and if they make a complaint, they fear it may result in being sent home,” McLaughlin said.
McLaughlin, whose research examines health and human rights issues of migrant farm workers, said that in addition to the fear of repatriation, other issues such as language barriers, proximity to clinics and migrant worker illiteracy hinder access to health care.
And many workers — Morrison among them — simply don’t go to the doctor often. Morrison admits that until his initial leg injury, which later led to his amputation, he hadn’t been seen by a doctor for 10 years.
When Morrison arrived in Leamington, Ontario, in 2004, he was no stranger to farm work. In Jamaica, the 38-year-old had been raising livestock and growing citrus fruit. Like all recruits for Canada’s guest worker program, he underwent a series of required medical screenings for illnesses that could be contagious, including HIV.
While Canada requires these medical screenings for guest workers, there is no requirement between Canada and the sending countries for medical screenings before the workers return home.
“The purpose of the exam isn’t to ensure the worker’s welfare, the purpose is to ensure that Canadian employers are receiving healthy workers and that the Canadian healthcare system won’t be burdened with complex health problems of these workers, and that Canadian public health won’t be compromised through the spread of infectious disease,” said McLaughlin, who has done extensive research on Canada’s guest worker program.
Morrison believes that if he had received some sort of medical screening prior to leaving Canada, it would have saved his leg from amputation.
“Just like when I come from Jamaica, and they have to do a test, then you should have a system when I’m going back home, you do that same test to show that I’m going back to my family safe without anything," Morrison said. "If I could not come here sick, then I should not come back to my country sick."

Morrison looks at photos of his family during an interview at the Worker's Action Center in Toronto. Due to a workplace injury that led to amputation of his leg, Morrison can no longer do agricultural work. He is now an advocate for Canada's guest workers. Photo by Lillian Reid. |
Morrison’s saga began in June 2011 when he was spraying pesticides in a greenhouse and he slipped and fell injuring his right femur. Morrison said he was told by a doctor at a nearby health clinic that it was a pulled muscle, and that he would need to come back regularly for check-ups on his knee. Three months later, he had surgery on his knee and a steel plate was put in.
At that point, all of his medical expenses were paid. In Canada’s Seasonal Agricultural Worker Program, every worker, who is injured on the job, is covered with a form of worker’s compensation insurance by the Workplace Safety and Insurance Board.
But Morrison’s knee continued to bother him after the seasonal work was done and by contract, he returned to Jamaica.
His knee injury worsened to the point he felt it necessary to return to Canada for further treatment. Before he left Canada, Morrison’s doctor told him that if he needed to return for treatment, all he needed was a letter from his doctor in Jamaica.
However, Morrison’s doctor in Jamaica didn’t give him the letter. He sought a second opinion and the doctor found that he now had a tumor in his knee and needed to return to Canada for treatment.
When the Workplace Safety and Insurance Board found out about the tumor, they cut off his worker’s compensation for eight months, Morrison said. He explained he was told by the WSIB that it would no longer cover his medical expenses because his tumor was not a result of a workplace injury and that he had cancer, when he in fact didn’t.
Unfortunately, Morrison said that by the time the dispute was settled and he returned to Canada, a serious infection had developed from the plate in his knee, which resulted in the amputation of his leg in May 2012.
Several attempts were made to contact WSIB officials for a response regarding Morrison’s case, but they refused to comment. However, Morrison said the WSIB is now covering his expenses for physical therapy and mental health treatment.
Morrison isn’t certain how the tumor in his leg developed. He postulated that pesticide exposure might have had something to do with it since the bunkhouse where workers slept was built directly on top of the greenhouse where tomatoes were grown and sprayed with pesticides.
“I was in my bunkhouse more than one time and the chemicals they spray in the greenhouse were coming upstairs through the vent," he said. "And guys would start to feel bad, they have to call the boss and put everybody outside, because all the fumes were coming out from the greenhouse."
Throughout Morrison’s ordeal with his injury and leg amputation and dealing with WSIB he said that his Jamaican liaison service did nothing to help expedite his surgery. Within Canada's guest worker program, workers have a liaison officer from their country who acts as a mediator if a dispute should arise between the employer and the worker.
In fact, shortly after Morrison received the first surgery on his knee, he said the liaison service forced him to return to Jamaica, even though he couldn’t walk properly. He believes he should have been allowed to stay in Canada until he fully recovered.
“My liaison service tried to push me out to Jamaica, and I said, ‘I just had my surgery I cannot walk, I cannot do anything and you’re trying to get me out to Jamaica? What’s going to happen to me?’" Morrison said. He then refused to go, but he said his liaison told him he would be reported to the Canadian government as missing.
In 2012, the Toronto Star reported from Canadian government statistics that between 1996-2011, 3,709 migrant workers in SAWP have been deemed AWOL (absent without leave) and 1,198 were sent home for medical reasons. Morrison was never deemed AWOL, but he took the comments as a threat that he could be falsely accused.
Several attempts were made to contact the office of the Jamaican secretary of labor regarding protections for their workers, but there was no comment.
Morrison’s experience in Canada’s SAWP is one of the more extreme cases but it highlights many of the concerns workers, their advocates and researchers have raised about healthcare within the program.
McLaughlin said liaison officers are wary about advocating too strongly for fear employers will cancel contracts with the country.
“Their power is very limited because if the employer is unhappy with the worker, they can fire the worker and they can even fire the entire workforce from that liaison officer’s country, so many liaison officers would say, ‘My primary job is to protect the jobs of the workers and by doing that I don’t want to raise my voice too high and complain on behalf of the workers because that might result in all of the workers losing their job,’” McLaughlin said.
As the U.S. debates immigration reform, the leading bipartisan proposal for a guest worker program does not include a provision requiring health care for guest farm workers, but it would require worker’s compensation insurance.
For workers in the U.S. who do not have health care insurance, there are few options to treat sickness or injury. Farm workers are covered for work-related injuries and disease through worker’s compensation. However, they often turn to self-medication or go to free clinics to treat outside-of-work illnesses. If those two options aren’t possible, then workers frequently go to emergency rooms, the most expensive form of healthcare.
An alternative to seeing workers in the emergency room is to take primary care clinics to workers, said Anne Passalugo, director of emergency management in community programs at Niagara Falls Memorial Medical.
For the past five years, the hospital has run a federally funded program using mobile clinics to provide free medical services to migrant farm workers in the Niagara Falls, N.Y. area. Passalugo said the majority of patients who come to the clinics have a need for less urgent, less serious services.
Passalugo said that if more focus were placed on providing free primary care services to migrant farm workers, then the issue of high cost emergency room visits would lessen.
“A way around it could be doing a program such as ours on a weekly basis, or even two or three times a week where programs are created where they could go out and provide primary care to these individuals because most of the time what we’re seeing…they’re not acute problems,” said Passalugo.
Passalugo said the focus should not be on insurance, but on delivering primary healthcare to the workers, which would keep them out of emergency rooms.
For Morrison, the dispute over who would pay for his health care cost him a leg. He currently remains in Ontario where he is getting physical therapy and working alongside Justicia 4 Migrant Workers.
Although Morrison is no longer physically able to do farm work, he remains in Ontario to advocate for farm worker rights. Throughout his ordeal, Morrison credits his love for his children and his faith in God as the only things that have kept him sane.
Back to Top
